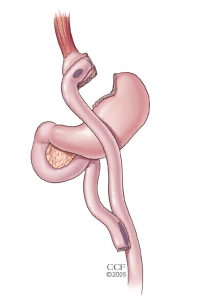
RNY Gastric Bypass
About the procedure:
In this procedure, the top portion of the stomach is stapled off from the natural stomach creating a small (1 ounce) stomach pouch. The remainder (remnant) of the stomach is not removed, but is stapled and cut away from the stomach pouch. Portions of the small intestine are re-rerouted in a “Y” shape. The outlet from the newly formed 1 ounce pouch is sewn directly to the new small intestine resulting in early satiety and reduced absorption of food, nutrients and vitamins. Bypassing the remnant stomach causes a marked decrease in ghrelin production and a lack of hunger. The lack of hunger usually lasts for 6 months to two years. Vitamin and nutrient absorption are significantly reduced and some medicines are not well tolerated after the procedure.
How It Works:
1. The small gastric pouch restricts meal volume, but more importantly, it allows early and prolonged satiety. Patients feel full with a small amount of food, and they are not hungry or looking for food between meals.
2. Bypassing the remnant portion of stomach decreases production of the hunger hormone ghrelin which markedly reduces hunger for a long time.
3. Bypassing the remnant stomach and some of small intestine provides impaired absorption of nutrients that a patient consumes.
4. The dumping syndrome (cramping abdominal pain after eating carbs and sweets) occurs in two out of three patients reminding those patients to eliminate carbohydrates from their diet.
Indications:
The gastric bypass is indicated for use in weight reduction for severely obese patients with a Body Mass Index (BMI) of at least 40 or a BMI of at least 35 – 39 with one or more severe co-morbid conditions, or those who are 100 lbs. or more over their estimated ideal weight. A patient with a BMI of 40 usually weights about 100 lb above their ideal body weight.
Malabsorption:
Yes. The absorption of most vitamins minerals and nutrients are decreased after the gastric bypass.
Vitamin Requirement:
Three daily multivitamins, B12, folic acid, Calcium iron and Vitamin D should be taken should be taken for the rest of a person’s life due to the malabsorption of gastric bypass.
Dietary Restrictions:
Patients may experience dumping syndrome with intake of carbohydrate foods.
A condition known as “dumping syndrome” occurs as the result of rapid emptying of stomach contents into the small intestine. This is often triggered when too much sugar or large amounts of food are consumed. While generally not considered to be a serious risk to your health, the results can be extremely unpleasant and can include nausea, weakness, sweating, fainting, and on occasion, diarrhea after eating. Most patients are unable to eat any form of sweets after surgery without experiencing dumping syndrome. A low carbohydrate diet enhances the effectiveness of this procedure.
Laparoscopic:
Yes
Number of incisions:
5
Intestinal Rerouting:
Yes
Cutting or stapling:
Yes – Stomach Wall and small bowel
Hospital Stay:
Inpatient – Patients usually stay 1 night in the hospital
Recovery:
Most patients return to normal activity in two weeks. Full surgical recovery occurs in two to three weeks.
Post Op Diet:
As with all surgical weight-loss programs, it is imperative that gastric bypass patients adhere to a strict postoperative diet. Patients must stick to a liquid protein diet for 3 weeks after surgery. Patients then graduate to a soft protein based diet for 2 weeks and then at 8 weeks, patients transition to a low carb solid diet. Once goal weight is achieved, usually 2-3 years after surgery, most patients consume a normal healthy diet with the appropriate number of calories for their height and build to maintain their weight.
Mortality:
The risk of mortality during the first 30 days following surgery with the gastric bypass is 0.5-1% (less than one out of every 100 patients die from the procedure). We have never had a peri-operative death following gastric bypass surgery.
Hair Loss:
Patients may experience hair loss during period of rapid weight loss. Hair growth does not always normalize with weight maintenance as it can be a side effect of nutritional deficiencies related to malabsorption of critical nutrients.
Bone Disease or Osteoporosis:
Patients are at increased risk as a result of malabsorption of critical nutrients.
Bypassing the duodenum has caused metabolic bone disease in some patients, resulting in bone pain, loss of height, humped back, and fractures of the ribs and hip bones. Women already at risk for osteoporosis that can occur after menopause, should be aware of the potential for severe bone calcium loss. All of the deficiencies mentioned above must be managed through proper diet and vitamin supplementation.
Iron Deficiency Anemia:
Patients are at increased risk as a result of malabsorption of critical nutrients.
Because the duodenum is bypassed, poor absorption of iron and calcium can result in the loss of total body iron and a predisposition to iron deficiency anemia. This is a particular concern for patients who experience chronic blood loss, excessive menstrual flow or bleeding hemorrhoids.
Reversible?:
Technically difficult to reverse, however, it is possible to rejoin the stomach sections, and reposition the small bowel. The stomach and small bowel will never function as they did before surgery.
Easily Adjustable:
No. The gastric bypass can only be adjusted through an additional surgical procedure.
Pregnancy:
It is not recommended that you become pregnant during the weight loss period following a gastric bypass, as women are often malnourished. Weight loss after gastric bypass occurs because the patient cannot intake enough nutrition to support themselves, rendering them incapable of providing adequate nutrition to support a developing baby.
Contraindications:
The RNY Gastric Bypass is not recommended for non-adult patients (will be evaluated on a case-by-case basis), patients with conditions that may make them poor surgical candidates or increase the risk of poor results, who are unwilling or unable to comply with the required dietary restrictions and vitamin supplementation, or who currently are or may be pregnant. Patients with osteopenia or osteoporosis are excluded from possible gastric bypass candidates due to malabsortion of necessary Calcium and Vitamin D supplementation.
Weight Loss:
Typical patients lose weight at a rate or 2-3 pounds per week. Weight loss is rapid but usually slows by twelve to eighteen months post op.
One year after surgery, weight loss averages to 77% of excess body weight.
Studies show that after 10 to 14 years, 50-60% of excess body weight loss is expected.
